Some surprises are nice.
Winning tickets to a great concert.
Finding $20 in the pocket of a coat you haven’t worn in a year.
Your significant other bringing home chocolate.
Some surprises are not so nice.
A mouse running past you in the basement.
Running into someone unpleasant from your past.
Surgery!
Bet you can guess which surprise I got!
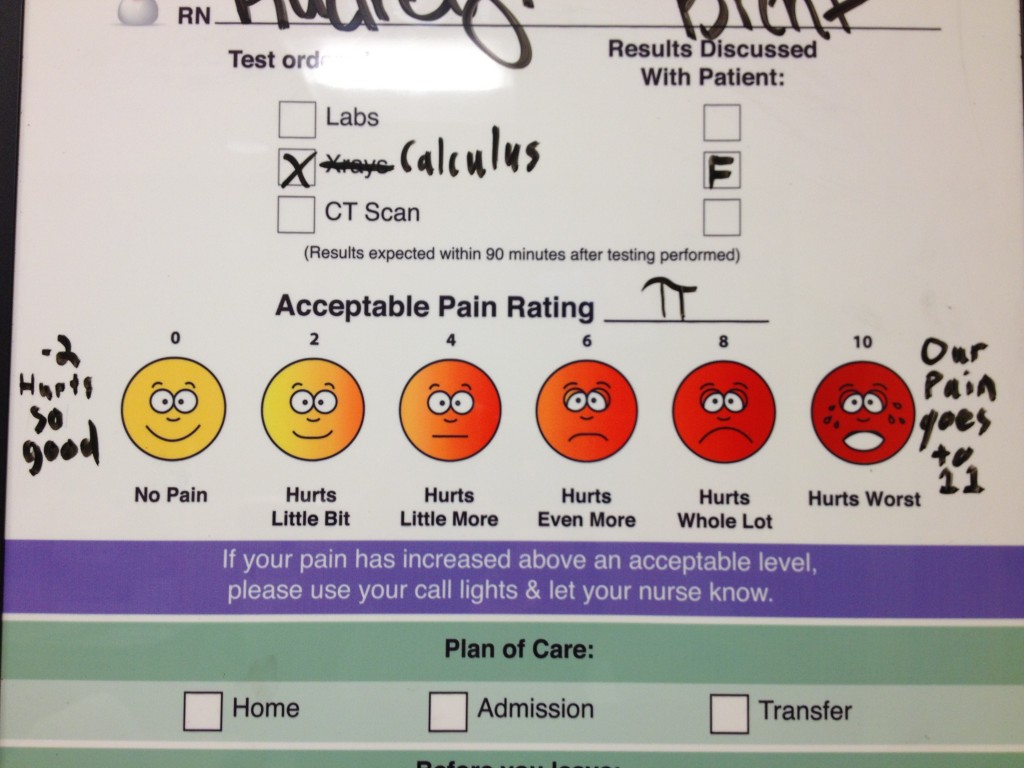
Friday I woke up to some abdominal pain around my umbilical hernia. It wasn’t bad, just a little sore, so I didn’t think too much about it. Saturday morning I woke up and it was worse. Within a couple of hours, shortly after breakfast, the pain was almost unbearable. I texted Mark, who was running errands, to come home. I could barely get myself dressed and get together stuff for the boys. My whole body felt flushed and I couldn’t stand up straight. I’d never felt the pain before, but I recognized the symptoms of a strangulated hernia.
At the local ER, the doctor attempted to push my intestines back where they belonged. Without giving me pain meds. I don’t recommend this. I cried a lot. One CT scan later the doctor explained that while he’d gotten most of my intestines back in, one bit remained and blood supply was being cut off, so I would need emergency surgery. He called it an incarcerated hernia and assured me that the surgical team would be waiting for me at the main hospital’s ER.
Of course, that wasn’t the case. It took a couple of hours for anyone from surgery to come to see me, and that person ended up being a resident who palpated my abdomen and said that I probably didn’t have any intestines trapped, just fat, and that I could probably go home. Mark and I weren’t comfortable with that (I mean, I was on morphine and still yelling in pain), so the resident said she’d talk to her attending about admitting me and doing surgery Sunday or Monday, and that she’d be back. 6 hours after I’d arrived at the second ER (12.5 hours after I’d arrived at the local ER) I was finally put in a room. It was about 1:30 am. At this point I’d not seen a surgical attending, the resident had never come back, and some random ER resident told me that I was never having surgery and that the only reason the surgeon thought it was fat trapped and not intestine like I’d been told is because I wasn’t have enough pain. I was not pleased and politely demanded to talk to someone from the surgical team. Unfortunately, that was another resident and she wasn’t able to answer my questions, other than to say I didn’t need surgery.
Now, as an aside, I knew that if I had to have surgery it needed to be this week. It just so happened that my mother-in-law’s knee surgery was supposed to have been Friday but was canceled last minute. There was family visiting in town to be able to help with the kids. If done now, I might be recovered in time to still attend the NMF gala and board retreat in a few weeks. Plus, if surgery was delayed a few weeks, my MIL and I would be recovering at the same time, when Mark and I were planning on being able to help her a lot.

I wasn’t allowed to shower, so I was given a magic shower cap with shampoo, conditioner, and water all mixed in. It sounds gross, but it actually cleaned my hair pretty well!
Sunday morning a third surgical resident came by, with the same demeanor the other two had had…a kind of “why are you taking up our hospital space” attitude. He was the first to explain what surgery would entail, though he insisted that would take place in a few weeks: pain for about a week, then an additional 3 weeks of not being able to life 5-10 lbs. I just cried for a good while after he left, because I had NOOO idea how I’d ever get that to work. I know I’m not supposed to lift over 20 lbs anyway, since I have Marfan, but I pick up both of those kids multiple times a day.
FINALLY the attending surgeon came to see me. He said he was going to try to operate on me that afternoon. So much for the residents knowing anything!
I ended up not having surgery till Monday, and with a different surgeon than originally planned. The lack of communication from the surgical department was really frustrating…they just flat out did not return pages from either the ER docs on Saturday, or the nurses on the surgical floor on Sunday. The surgeon I was paired with had never operated on someone with Marfan before, which is obviously less than an ideal situation. We discussed her plan for my hernia, and she had decided against using mesh, which is the standard of care for Marfan patients. However, what I liked about this surgeon is that she was willing to discuss everything with me. She explained that because the hernia was so small (small umbilical hernias cause more problems than large ones, because with large ones the intestine or tissue slides right back instead of getting stuck), she could close it with just a couple of stitches. If she put in mesh, the healing time would be longer and there would be an increased risk of adhesion complications. I have a personal history of serious adhesion complications. So, I agreed that her plan made sense, but requested she put in extra stitches to try to get the repair to hold, and she agreed that my request made sense.
She gives the surgery an 80% chance of holding (for typical people), and I’d guess it’s a bit less for those of us with Marfan. I’m bound and determined for this surgery to work, so I’m really trying to take it easy.
Surgery itself went well. I had some premature atrial contractions during surgery, but those are not anything to worry too much about. Most of the nurses I had were excellent, maybe the best nursing experiences I’ve had. But, the hospital was definitely understaffed. It was hard to manage pain when it would take an hour to get my meds. I intend to give my feedback to the hospital. It really stinks for such great nurses to not be able to do their jobs effectively if the hospital won’t back them up by ensuring there are enough nurses on the floor.
I got home yesterday afternoon. I’m feeling pretty dizzy, I think from the pain meds, but other than that doing ok. Going to take it very easy so that I can hopefully make it on my NYC trip in 3 weeks. Cross your fingers, please!



10 Comments
Leave a reply →